J'S AI Platform
Computer-Assisted Coding Services
Computer-Assisted Coding Services to accelerate your revenue cycle with AI precision.
Trusted by 1000+ Companies


















We Simplify Your Ops and Revenue Cycle through meticulous Computer-Assisted Coding Services
At J’S Vision Code, we help healthcare providers simplify and improve their medical coding process. Our team combines skilled coders with computer-assisted coding (CAC) tools to turn clinical records into accurate billing codes. This not only reduces manual errors but also speeds up claim processing and supports cleaner, faster reimbursements. From hospital systems to outpatient clinics, we make sure your coding stays consistent, reliable, and fully aligned with current healthcare standards.
Our Computer-Assisted Coding Services
CAC Setup and Documentation Review
Real-Time CAC at Point of Care
Post-Visit CAC Review
EHR Integration and Data Abstraction
Audit and Compliance Support
Analytics and Reporting
Code Validation with CMS Guidelines
Support for Medicare Advantage and Risk Adjustment
Hybrid Coding for ACOs and Population Health
Our Signature Process
An AI-First Approch
Before coding begins, our system checks that all clinical records are complete, properly formatted, and ready for processing. We verify patient information, coverage details, and documentation quality to reduce coding delays and errors. This early validation step improves coding accuracy and helps your team stay ahead of claim cycles.

Using advanced CAC tools, we scan clinical notes and automatically suggest ICD-10-CM, CPT, and HCPCS codes. Our certified coders then review each suggestion, applying coding guidelines and documentation standards to confirm accuracy. Each chart goes through a secondary check to ensure the final codes are audit-ready and fully compliant.

Once the codes are finalized, we prepare the files for direct submission into your billing or practice management system. This includes creating detailed records with supporting notes and encounter data. Our process helps speed up claim submission, reduce manual handoffs, and minimize the risk of rework or rejections.

Our tools use natural language processing (NLP) and intelligent automation to read and understand clinical language. They flag missing diagnoses, detect possible documentation issues, and highlight areas that need human review. This smart system improves consistency, lowers chart review time, and provides a clear audit trail for every action.
We provide live dashboards that show code accuracy rates, productivity metrics, documentation gaps, and coder review trends. With these insights, your team can improve coding workflows, address problem areas, and stay aligned with quality goals. The result is better reporting, smoother operations, and stronger financial performance.
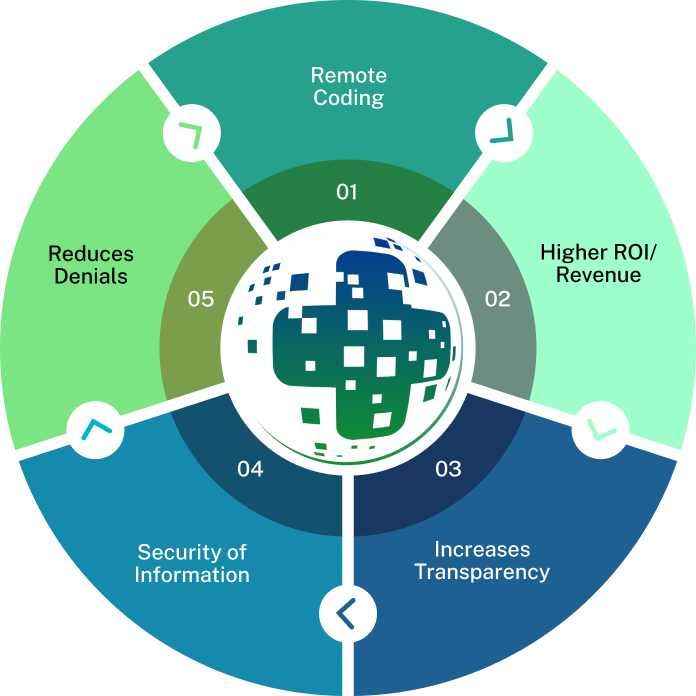
Why Choose J’S Vision for Facility Coding Services?
Here’s why so many health plans and provider groups trust J’S Vision for their Facility Coding Services:
We make coding easier and faster
Our AI-powered CAC system automatically reads charts and suggests accurate ICD-10, CPT, and HCPCS codes. This reduces manual work, speeds up coding, and gives your team more time to focus on patient care.
Every code is backed by expert review
Each suggestion from our CAC tool is reviewed by certified coders who follow the latest CMS and payer guidelines. This ensures that every diagnosis is coded correctly and completely.
Problems are caught before they become denials
Each chart passes through multiple checkpoints, including peer review and manager oversight. Our quality assurance process helps you reduce claim errors and protect your revenue.
Flexible options for different coding needs
Whether you need real-time support during the care process or a detailed audit of past records, we offer both prospective and retrospective coding workflows to suit your team’s preferences.
Real-time reports to guide your next steps
Our dashboards give you a clear view of RAF trends, denial rates, and coding accuracy. You can monitor team performance, spot gaps, and make informed decisions quickly.
Secure, scalable, and EHR-ready
Our platform works with your existing EHR through standard integrations. It is fully HIPAA-compliant and built to scale with your organization, whether you’re a small clinic or a national payer.
Support that grows with your team
Your dedicated account manager checks in regularly, offers personalized advice, and ensures your team stays updated on all changes in medical coding guidelines.
Trusted Partners
Relate is a better way to do sales and customer success for B2B SaaS startups

“The team at J’S Vision delivers our coding files on schedule with very few errors. We trust them for both outpatient and inpatient work so we do not have to double check. That saves us hours each week.”
Dr. Raj Malhotra Chief Medical Officer
“Working with J’S Vision feels like having our own coding department on call. They answer questions right away and update any files that need fixes. Their reliable service keeps our billing on track and makes audits smoother.”
Kara Simmons Practice Administrator
“J’S Vision handles our toughest cases such as emergency visits and long term care with skill and care. Their notes are always clear so we rarely have to ask for more detail. Our staff now spends less time on paperwork and more time with patients.”
Thomas Griggs Operations Manager
“With J’S Vision, audit flags are a thing of the past. Their coding is correct the first time and they turn around any revisions within a day. Our audit scores have gone up and we have real peace of mind.”
Lisa DuPont Compliance & Quality Officer
“The team at J’S Vision cleared our coding backlog and cut our billing cycle by two days. We have seen a steady rise in processed claims and a drop in manual rework. Our finance team loves their simple easy to read reports.”
Jordan Lee Billing and Claims Lead
Book a Free 30-Minute Consultation with Our Computer-Assisted Coding Specialists
Some issues we can discuss are:
How your current coding process works and where CAC can fit in
Common issues causing claim denials or delayed submissions
How automation and NLP tools can improve coding speed and accuracy
Ways to improve HCC scoring accuracy and align with CMS requirements
Whether you're just getting started with CAC or looking to upgrade your system, our team will guide you through your options and help you move forward with clarity.
Food for your Thoughts




“J’S Vision’s accurate coding cut our claim denials by half, and it freed our billing team to spend more time on patient care. Their clear reports show exactly where to fix issues. We receive payment faster with fewer questions.”
Emily Tran Director of Revenue Cycle Management