J'S AI Platform
Computer-Assisted Professional Coding Services
Rapid AI Suggestions, Rigorous Human Validation
Trusted by 1000+ Companies


















We Simplify Your Practice’s Medical Coding with AI’s speed and Human validation.
At J’S Vision, we bring together advanced AI coding tools and the expertise of certified medical coders to make claim submissions faster and more accurate. Our Computer-Assisted Professional Coding service reviews clinical documentation in real time, suggests ICD-10, CPT, and HCPCS codes, and then has our specialists confirm each code so it truly reflects the patient’s story. This approach cuts down denials, strengthens compliance, and creates a smoother workflow that lets your team focus on what matters most delivering excellent patient care.
Our Computer-Assisted Coding Services
Multi-Format Data Ingestion & Prep
Clinical NLP & Entity Extraction
Knowledge Graph & Ontology Mapping
Deep Learning Code Prediction
Rule-Engine Edits & Validation
Confidence Scoring & Autonomous Coding
Integrated Coder Workflow
EHR & API Connectivity
Analytics & Continuous Learning
Compliance & Security
Our Signature Process
An AI-First Approch

We pull structured HL7 v2/v3 feeds, FHIR R4 resources, free-text notes and OCR’d scans into our platform. Layout normalization, de-duplication and PHI-stripping modules then segment clinical sections (HPI, ROS, Assessment/Plan) to ensure clean input for our coding engines.

Our NLP pipeline tokenizes text, detects negation and extracts clinical entities. Transformer-based models predict ICD-10-CM, ICD-10-PCS, CPT and HCPCS codes while a rules engine applies NCCI/CCI edits, Excludes1/2 checks and bundling logic to flag conflicts before human review.

Certified coders work in an integrated UI where each AI-suggested code carries a confidence score. Coders accept, modify or reject suggestions with one click. Built-in query tools generate clinician queries when documentation gaps arise, ensuring every code matches true clinical intent.

Native HL7, FHIR and SMART on FHIR connectors sync with Epic, Cerner, Meditech and other systems. Approved codes flow automatically into your RCM and billing modules, eliminating manual entry, accelerating charge capture and reducing downstream denials.

Real-time dashboards track suggestion accuracy, charts per hour, denial rates and audit exceptions. Coder edits and audit feedback feed into regular ML retraining and rule-set updates, driving ongoing gains in precision and productivity.
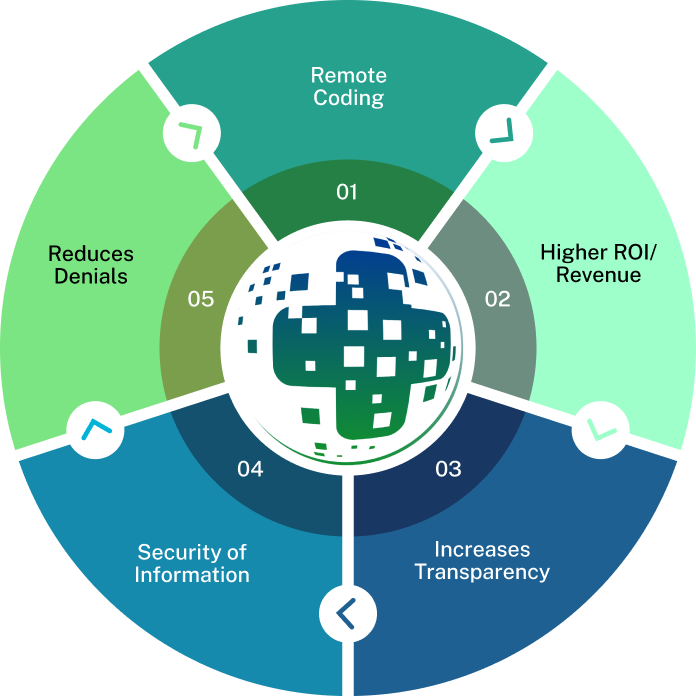
Why Choose J’S Vision for Computer-Assisted Coding?
Here’s why healthcare providers and health plans trust J’S Vision Code to improve their medical coding with advanced computer-assisted coding technology:
We lighten the coder’s workload
Our AI-driven NLP and machine-learning tools pre-process clinical notes, identify key diagnoses and procedures, and suggest accurate ICD-10, CPT and HCPCS codes so your team can work faster.
Expert review for every code
Every AI-generated suggestion is validated by AAPC- or AHIMA-certified coders who follow the latest CMS, AMA and payer-specific guidelines to ensure total compliance.
Three layers of quality control
Codes with high confidence scores are auto-approved, mid-level scores go through peer review and low-level scores receive manager validation to catch every potential error.
Flexible to match your workflow
Whether you need real-time, point-of-care support or retrospective batch audits, our platform adapts to your process and uncovers missed coding opportunities.
Real-time analytics and insights
Interactive dashboards display code suggestion accuracy, coder productivity, denial drivers and rule-exception trends so you can optimize performance instantly.

Seamless, secure integration
Native HL7, FHIR and SMART on FHIR connectors integrate with Epic, Cerner, Meditech and more while enforcing HIPAA-grade security and role-based access controls.
A true partnership approach
From initial setup and coder training to ongoing model retraining and rule-set updates, your dedicated account lead collaborates with you to drive continual improvement.
Trusted Partners
Relate is a better way to do sales and customer success for B2B SaaS startups

“The team at J’S Vision delivers our coding files on schedule with very few errors. We trust them for both outpatient and inpatient work so we do not have to double check. That saves us hours each week.”
Dr. Raj Malhotra Chief Medical Officer
“Working with J’S Vision feels like having our own coding department on call. They answer questions right away and update any files that need fixes. Their reliable service keeps our billing on track and makes audits smoother.”
Kara Simmons Practice Administrator
“J’S Vision handles our toughest cases such as emergency visits and long term care with skill and care. Their notes are always clear so we rarely have to ask for more detail. Our staff now spends less time on paperwork and more time with patients.”
Thomas Griggs Operations Manager
“With J’S Vision, audit flags are a thing of the past. Their coding is correct the first time and they turn around any revisions within a day. Our audit scores have gone up and we have real peace of mind.”
Lisa DuPont Compliance & Quality Officer
“The team at J’S Vision cleared our coding backlog and cut our billing cycle by two days. We have seen a steady rise in processed claims and a drop in manual rework. Our finance team loves their simple easy to read reports.”
Jordan Lee Billing and Claims Lead
Request a Free 30-Minute Consultation With Our Computer-Assisted Professional Coding Specialists Today!
Some issues we can discuss are:
Your existing CAPC workflows and system architecture
Common coding and billing errors and how AI flags them
Strategies to boost accuracy and throughput with NLP/ML automation
Best practices for seamless EHR/API integration and real-time code delivery
Continuous-learning frameworks, analytics dashboards, and audit readiness
Food for your Thoughts




“J’S Vision’s accurate coding cut our claim denials by half, and it freed our billing team to spend more time on patient care. Their clear reports show exactly where to fix issues. We receive payment faster with fewer questions.”
Emily Tran Director of Revenue Cycle Management