Services
Facility Coding Services
Maximize Revenue, Minimize Denials
Trusted by 1000+ Companies


















We streamline your facility coding for maximum accuracy and reimbursement.
Our expert facility coding team ensures precise and compliant coding for all facility-based services including inpatient, outpatient, and emergency care. We manage the entire coding process so your internal teams can stay focused on operations and patient care. Each encounter is carefully reviewed to ensure accurate assignment of CPT, ICD-10, and HCPCS codes. Our AI-powered validation tools identify inconsistencies and highlight documentation gaps that need attention. You receive detailed, audit-ready reports along with insights to reduce denials and improve revenue capture. This service supports regulatory compliance, minimizes billing errors, and helps your facility secure full and timely reimbursement.
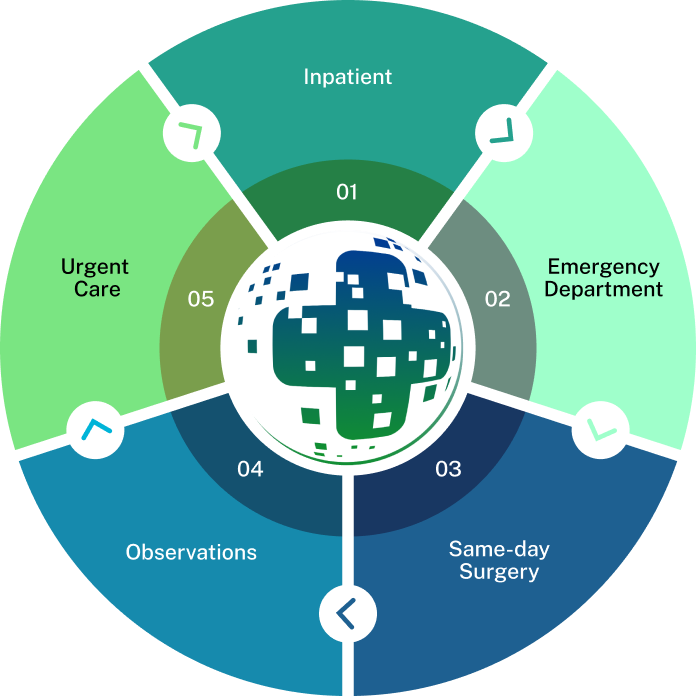
Our Comprehensive Facility Coding Services
Inpatient & Outpatient Coding
Emergency Department (ED) Coding
Ambulatory Surgery Center (ASC) Coding
Radiology & Pathology Coding
Denial Management & Auditing
Charge Capture & Revenue Integrity
Our Signature Facility Coding Process
An AI-First Approch

Before coding begins, we validate patient eligibility and encounter type using integrated clearinghouse systems and payer-specific criteria. Our process verifies insurance coverage, service authorizations, and facility-level billing rules to ensure claims meet CMS, Medicaid, and commercial payer guidelines. This front-end verification minimizes denials and maximizes first-pass claim acceptance.

Certified facility coders review provider documentation and clinical records to assign accurate ICD-10-CM, CPT®, and HCPCS Level II codes. We apply MS-DRG, APC, and status indicator logic appropriate to the place of service (IP, OP, ED, ASC). Coding adheres to official coding guidelines, payer bulletins, and NCCI edits. Every record undergoes dual-level review to ensure clean claims, optimize case mix index (CMI), and support compliant billing.

We convert coded data into complete UB-04 claim forms using revenue code mappings, charge descriptions, and condition/value codes where applicable. Claims are scrubbed using proprietary edits and payer-specific logic, then submitted electronically under HIPAA-compliant protocols. Submission tracking ensures timely follow-up and resolution of payer rejections or edits.

Using Natural Language Processing (NLP) and Robotic Process Automation (RPA), our platform flags undercoded services, missing documentation, and code-to-diagnosis mismatches. AI tools assist in mapping services to correct revenue codes and identifying gaps in provider notes. This improves documentation integrity, enhances coding productivity, and reduces downstream denials.

We provide clients with real-time access to dashboards tracking coding turnaround time, accuracy, denial trends, and revenue impact. Key Performance Indicators (KPIs) such as Clean Claim Rate, CMI shifts, and DRG mismatches are monitored to guide continuous process improvement. Analytics also identify patterns in medical necessity denials and outpatient edits, enabling proactive resolution.

Our compliance team conducts concurrent and retrospective DRG validation and supports internal and payer audits including RAC, MAC, and QIO reviews. We maintain full audit trails with coder rationale, source documentation, and change history. Our audit response process reduces risk exposure and ensures that your facility remains aligned with CMS, OIG, and state-level regulations.
Why Choose J’S Vision for Facility Coding Services?
Here’s why so many health plans and provider groups trust J’S Vision for their Facility Coding Services:
Certified Coding Experts
Our team is made up of AHIMA- and AAPC-certified coders with deep specialization in ICD-10-CM, CPT, and HCPCS Level II coding. Whether it’s inpatient DRG assignment, outpatient APC grouping, or ED-specific coding, we bring unmatched technical expertise to every encounter.
Three Layers of Quality Review
Every coded chart goes through a multi-tiered validation process peer review, audit by a senior manager, and a final compliance check. This ensures accuracy, supports revenue integrity, and minimizes downstream denials.
Compliance & Audit Readiness
We maintain full alignment with CMS guidelines, HIPAA privacy rules, and payer-specific billing protocols. Our coding practices are audit-ready, with documentation trails that meet the highest regulatory standards including for RAC, MAC, and commercial payer reviews.
Seamless EHR Integration
Our solutions integrate with all major EHR platforms, including Epic, Cerner, Meditech, and Allscripts. This reduces administrative workload, eliminates duplicate documentation efforts, and supports clean, timely claim submission.
AI-Augmented Efficiency
Our platform uses AI-driven tools for chart abstraction and code suggestion, helping identify gaps, flag errors, and reduce coding turnaround times. Every suggestion is reviewed by certified coders to maintain accuracy and accountability.
Actionable Insights & Dashboards
We provide real-time dashboards and reporting on coding accuracy, claim acceptance rates, denial trends, and case mix index (CMI). These insights help drive informed decisions and continuous process improvement.

Dedicated Client Support
You’re assigned a dedicated account manager who understands your facility’s unique workflows. We offer tailored support for denial management, audit responses, and end-to-end revenue cycle optimization.
A Scalable, Secure Partner
Whether you’re a standalone ASC or a multi-hospital system, we scale with your needs. Our team is U.S.-based, operates under strict HIPAA compliance, and is structured to support high-volume environments without compromising quality.
Trusted Partners
Relate is a better way to do sales and customer success for B2B SaaS startups

“The team at J’S Vision delivers our coding files on schedule with very few errors. We trust them for both outpatient and inpatient work so we do not have to double check. That saves us hours each week.”
Dr. Raj Malhotra Chief Medical Officer
“Working with J’S Vision feels like having our own coding department on call. They answer questions right away and update any files that need fixes. Their reliable service keeps our billing on track and makes audits smoother.”
Kara Simmons Practice Administrator
“J’S Vision handles our toughest cases such as emergency visits and long term care with skill and care. Their notes are always clear so we rarely have to ask for more detail. Our staff now spends less time on paperwork and more time with patients.”
Thomas Griggs Operations Manager
“With J’S Vision, audit flags are a thing of the past. Their coding is correct the first time and they turn around any revisions within a day. Our audit scores have gone up and we have real peace of mind.”
Lisa DuPont Compliance & Quality Officer
“The team at J’S Vision cleared our coding backlog and cut our billing cycle by two days. We have seen a steady rise in processed claims and a drop in manual rework. Our finance team loves their simple easy to read reports.”
Jordan Lee Billing and Claims Lead
Request a Free 30-minute Consultation With Our Facility Coding Specialists Today!
Some issues we can discuss are:
Current inpatient, outpatient, ED, or ASC coding workflows and challenges
Common coding and billing errors that lead to claim denials
How AI and automation can improve coding speed and accuracy
Strategies for cleaner claims and reduced rework
Best practices for aligning with CMS, commercial payer, and NCCI guidelines
Custom reporting, audit readiness, and denial prevention tactics
Food for your Thoughts




“J’S Vision’s accurate coding cut our claim denials by half, and it freed our billing team to spend more time on patient care. Their clear reports show exactly where to fix issues. We receive payment faster with fewer questions.”
Emily Tran Director of Revenue Cycle Management