Services
Medical Code Auditing Services
Tactically Auditing Your Codes, Strategically Safeguarding Revenue.
Trusted by 1000+ Companies


















We Optimize Your Practice’s Coding Integrity and Compliance
Our team of certified auditors conducts end-to-end reviews of your coding processes, so your staff can focus entirely on patient care. We meticulously examine clinical documentation and assigned codes to uncover undercoding, overcoding, and documentation gaps. Leveraging AI-driven analytics and expert peer review, we deliver clear, actionable insights that strengthen compliance, reduce denials, and maximize appropriate reimbursement.
Our Comprehensive Medical Code Auditing Services
Internal and External Audits
Prospective Audits
Retrospective Audits
Compliance Audits
Focused Coding and Documentation Reviews
Audit Support
Data Analytics and Reporting
EHR and Coding System Validation
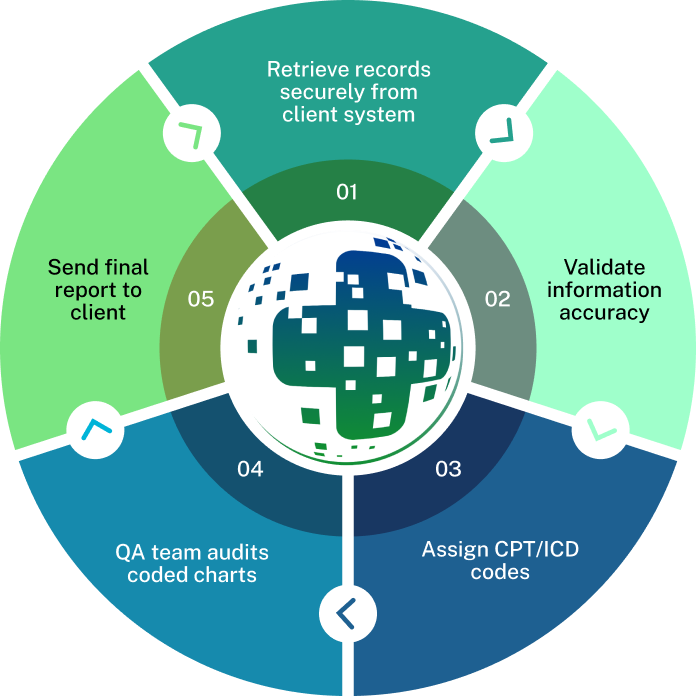
Our Signature Medical Coding Audit Process
An AI-First Approch

We begin with a collaborative kickoff workshop to define your audit’s scope, goals, and success metrics. By aligning objectives with your organizational priorities, whether that’s reducing denials, enhancing documentation, or ensuring compliance, we tailor our sampling strategy and timeline to fit your workflow. This phase also establishes clear reporting deliverables and stakeholder roles to keep the project on track.

Leveraging data-driven algorithms, we develop a statistically valid sample that balances random selection with targeted review of high-risk specialties and providers. Our risk stratification model assesses factors like claim volume, historical error rates, and payer-specific vulnerabilities to prioritize records with the greatest financial and compliance impact. This focused approach ensures efficient use of audit resources and maximizes recovery opportunities

Certified auditors meticulously compare clinical documentation to assigned ICD-10, CPT, and HCPCS codes, verifying that each code is supported by the medical record and adheres to payer and CMS conventions. We conduct multi-layered reviews, peer check, manager oversight, and final quality validation, to catch undercoding, overcoding, and modifier misuse. Any gaps are flagged for immediate feedback, reinforcing correct practices at the point of care.

Our AI-powered analytics platform scans audited records to detect patterns, outliers, and systemic coding anomalies in real time. By aggregating error types, such as insufficient documentation, incorrect code sequencing, or missing modifiers, we pinpoint root causes and quantify their financial impact. Interactive dashboards visualize trends, allowing your team to see where improvements will yield the highest return.

Upon audit completion, we deliver a comprehensive report that details error rates by provider, specialty, and code category, alongside prioritization of corrective actions. Each finding is accompanied by clear recommendations, educational resources, and workflow enhancement suggestions. We also conduct a debrief session to review results, answer questions, and co-develop a customized remediation roadmap.
To sustain progress, we implement an ongoing monitoring framework that re-audits key areas at defined intervals and tracks KPIs such as denial rates, coding accuracy, and documentation completeness. Quarterly check-ins and refresher trainings keep your team aligned with evolving regulations and internal quality benchmarks. This continuous feedback loop ensures lasting improvement and guards against future compliance risks.
Why Choose J’S Vision as Your Medical Code Auditing Services ?
Here’s why so many health plans and provider groups trust J’S Vision for their Medical coding auditing service:
Automated Audits
AI-powered platform automates chart reviews and code validation across specialties, reducing manual workload and identifying anomalies efficiently pre-submission.
Certified Accuracy
Certified auditors (CPC, CCS, RHIA) ensure accuracy and compliance with the latest ICD-10, CPT, HCPCS, and payer-specific guidelines.
Thorough Oversight
Three-tiered review process, peer checks, manager oversight, and final quality assurance, prevents undercoding, overcoding, and documentation gaps before claims submission.

Flexible Engagements
Flexible engagement models, prospective pre-billing audits, retrospective revenue recovery, and ongoing compliance monitoring, tailored to fit your operational needs and risk tolerance.

Visual Insights
Interactive dashboards visualize error patterns, denial drivers, and coder performance, empowering data-driven decisions to optimize revenue integrity and efficiency.
Secure Integration
Fully HIPAA-compliant infrastructure integrates seamlessly with any EHR or coding system, providing secure, scalable solutions for organizations of all sizes.
Ongoing Support
Dedicated account managers provide continuous training, performance reviews, and proactive compliance updates, ensuring your team stays aligned with evolving regulations.
Trusted Partners
Relate is a better way to do sales and customer success for B2B SaaS startups

“The team at J’S Vision delivers our coding files on schedule with very few errors. We trust them for both outpatient and inpatient work so we do not have to double check. That saves us hours each week.”
Dr. Raj Malhotra Chief Medical Officer
“Working with J’S Vision feels like having our own coding department on call. They answer questions right away and update any files that need fixes. Their reliable service keeps our billing on track and makes audits smoother.”
Kara Simmons Practice Administrator
“J’S Vision handles our toughest cases such as emergency visits and long term care with skill and care. Their notes are always clear so we rarely have to ask for more detail. Our staff now spends less time on paperwork and more time with patients.”
Thomas Griggs Operations Manager
“With J’S Vision, audit flags are a thing of the past. Their coding is correct the first time and they turn around any revisions within a day. Our audit scores have gone up and we have real peace of mind.”
Lisa DuPont Compliance & Quality Officer
“The team at J’S Vision cleared our coding backlog and cut our billing cycle by two days. We have seen a steady rise in processed claims and a drop in manual rework. Our finance team loves their simple easy to read reports.”
Jordan Lee Billing and Claims Lead
Request a Free 30-minute Consultation With Our Medical Code Auditing Specialists Today!
Some issues we can discuss are:
Your current coding audit processes and results
Common coding errors and denials in your practice
Strategies to reduce denials and reclaim revenue
Best practices for ongoing compliance monitoring
How AI and automation can streamline your audit workflow
Food for your Thoughts




“J’S Vision’s accurate coding cut our claim denials by half, and it freed our billing team to spend more time on patient care. Their clear reports show exactly where to fix issues. We receive payment faster with fewer questions.”
Emily Tran Director of Revenue Cycle Management