Services
Professional Fee Coding Services
Speed up provider reimbursements with accuracy, lower costs, and full compliance
Trusted by 1000+ Companies


















We streamline your professional fee coding for maximum accuracy and reimbursement.
Our expert facility coding team ensures precise and compliant coding for all facility-based services including inpatient, outpatient, and emergency care. We manage the entire coding process so your internal teams can stay focused on operations and patient care. Each encounter is carefully reviewed to ensure accurate assignment of CPT, ICD-10, and HCPCS codes. Our AI-powered validation tools identify inconsistencies and highlight documentation gaps that need attention. You receive detailed, audit-ready reports along with insights to reduce denials and improve revenue capture. This service supports regulatory compliance, minimizes billing errors, and helps your facility secure full and timely reimbursement.
Our Comprehensive Professional Fee Coding Covers
Expert Coders + Proprietary Workflow Tools
Emergency Visits
Multi-specialty E/M Coding
Hospital Medicine
Ambulatory Surgery
Anaesthesiology Coding
Ambulance Services
Pathology & Laboratory
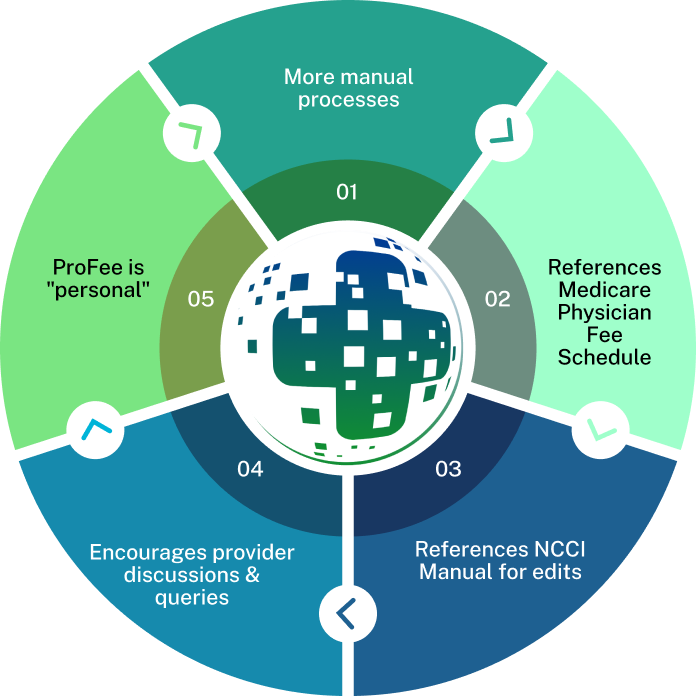
Our Signature Professional Fee Coding Process
An AI-First Approch

Before coding begins, we verify provider credentials, patient eligibility, and encounter specifics using integrated systems and payer-specific criteria. This ensures accurate assignment of services and compliance with CMS, Medicaid, and commercial payer guidelines.

Our certified professional coders meticulously review clinical documentation, including physician notes, operative reports, and diagnostic results. This thorough analysis ensures accurate capture of services rendered, supporting precise coding and billing.

Utilizing CPT®, ICD-10-CM, and HCPCS Level II code sets, our coders assign codes that accurately reflect the services provided. Special attention is given to Evaluation & Management (E/M) coding, ensuring adherence to the latest guidelines and payer requirements.

Leveraging advanced tools like Natural Language Processing (NLP) and Robotic Process Automation (RPA), we validate code assignments, identify discrepancies, and highlight documentation gaps. This technology-driven approach enhances coding accuracy and reduces the likelihood of denials.

We transform coded data into complete CMS-1500 claim forms, incorporating necessary modifiers and ensuring alignment with payer-specific billing rules. Claims are electronically submitted under HIPAA-compliant protocols, with tracking systems in place for timely follow-up and resolution of any rejections or edits.

Our compliance team conducts regular audits to ensure adherence to coding standards and supports responses to payer audits, including RAC, MAC, and QIO reviews. We maintain comprehensive audit trails, including coder rationale and source documentation, to support compliance and minimize risk exposure.
Why Choose J’S Vision for Professional Fee Coding Services?
Here’s why so many health plans and provider groups trust J’S Vision for their Professional Fee Coding Services:
Specialized Certified Coders
Our team of AAPC- and AHIMA-certified coders brings deep expertise across a wide range of specialties including E/M, surgery, hospital medicine, radiology, anesthesia, and more. Each coder is trained to apply nuanced professional fee coding rules, ensuring compliance with CMS, AMA, and payer-specific guidelines.
AI-Powered Validation & Workflow Tools
We leverage proprietary coding platforms integrated with Natural Language Processing (NLP) and Robotic Process Automation (RPA) to accelerate accuracy. These tools flag undercoding, overcoding, and documentation mismatches reducing the risk of audits and costly denials.
Rapid Turnaround Without Compromise
Our optimized workflows are built for speed and scale. Most charts are coded within 24-48 hours, even during peak volumes. You benefit from quick reimbursement cycles without compromising the accuracy or integrity of claims.
Denial Reduction & Revenue Maximization
We go beyond coding to help you improve financial performance. Our process includes proactive denial tracking, root-cause analysis, and claim correction strategies that reduce rework, capture missed revenue opportunities, and strengthen your bottom line.
Real-Time Reporting & Audit Readiness
With customizable dashboards, you gain visibility into coding productivity, accuracy rates, denial trends, and revenue impact. We maintain full audit trails with coder rationale and documentation links ensuring you’re prepared for internal reviews or external payer audits.
Scalable, Specialty-Agnostic Support
Whether you’re a single-specialty group or a large multi-site organization, our team scales with your needs. From ambulance to pathology, our coders seamlessly adapt to new providers, specialties, and EHR platforms delivering consistent, high-quality results.
Trusted Partners
Relate is a better way to do sales and customer success for B2B SaaS startups

“The team at J’S Vision delivers our coding files on schedule with very few errors. We trust them for both outpatient and inpatient work so we do not have to double check. That saves us hours each week.”
Dr. Raj Malhotra Chief Medical Officer
“Working with J’S Vision feels like having our own coding department on call. They answer questions right away and update any files that need fixes. Their reliable service keeps our billing on track and makes audits smoother.”
Kara Simmons Practice Administrator
“J’S Vision handles our toughest cases such as emergency visits and long term care with skill and care. Their notes are always clear so we rarely have to ask for more detail. Our staff now spends less time on paperwork and more time with patients.”
Thomas Griggs Operations Manager
“With J’S Vision, audit flags are a thing of the past. Their coding is correct the first time and they turn around any revisions within a day. Our audit scores have gone up and we have real peace of mind.”
Lisa DuPont Compliance & Quality Officer
“The team at J’S Vision cleared our coding backlog and cut our billing cycle by two days. We have seen a steady rise in processed claims and a drop in manual rework. Our finance team loves their simple easy to read reports.”
Jordan Lee Billing and Claims Lead
Request a Free 30-Minute Consultation With Our Professional Fee Coding Specialists Today!
Some issues we can discuss are:
Current E/M, procedural, and specialty-specific coding workflows and challenges
Common professional fee coding errors that contribute to denials or underpayments
How AI and automation enhance physician coding speed, accuracy, and compliance
Strategies for cleaner claims, accurate documentation capture, and reduced rework
Best practices for aligning with CMS, AMA, and payer-specific pro fee coding guidelines
Specialty-tailored reporting, audit readiness, and denial prevention strategies
Food for your Thoughts




“J’S Vision’s accurate coding cut our claim denials by half, and it freed our billing team to spend more time on patient care. Their clear reports show exactly where to fix issues. We receive payment faster with fewer questions.”
Emily Tran Director of Revenue Cycle Management