Services
Risk Adjustment Coding Services
Expert documentation and coding for complex cases and comorbidities.
Trusted by 1000+ Companies


















We Simplify Your Practice’s Risk Adjustment HCC Coding
Our team of certified coders manages every aspect of risk adjustment HCC coding, so your staff can devote their full attention to patient care. We meticulously review each medical record to assign accurate HCC codes and confirm completeness. Our AI-powered tools identify any documentation gaps and recommend updates, helping you maintain thorough records. You will receive detailed reports on risk scores along with clear guidance for strengthening clinical notes. This service meets payer regulations, lowers audit risk, and secures appropriate reimbursement for the care you provide.
Our Comprehensive Risk Adjustment HCC Coding Services
HCC Coding and Documentation Review
Prospective HCC Coding
Retrospective HCC Coding
Medical Record Retrieval and Abstraction
Audit Support
Data Analytics and Reporting
Hierarchical Condition Category (HCC) Validation
Medicare Advantage (MA) Risk Adjustment
Accountable Care Organization (ACO) Risk Adjustment
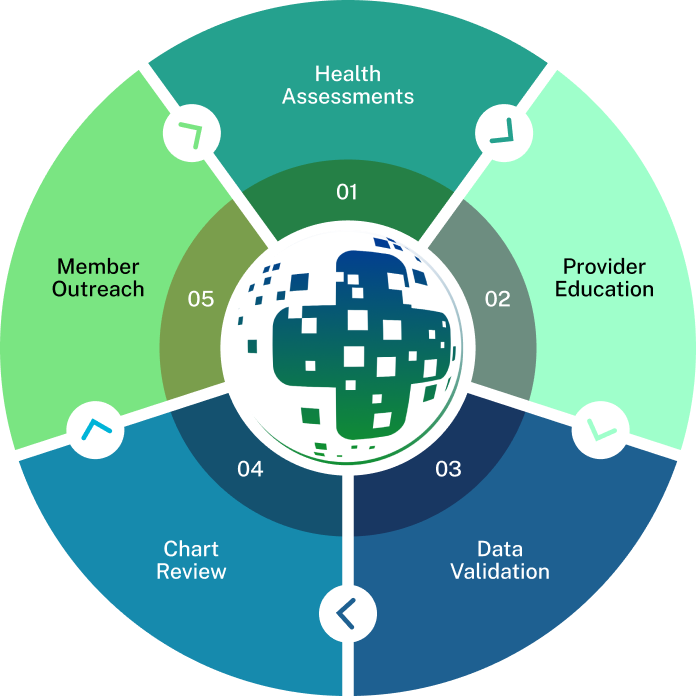
Our Signature Process
An AI-First Approch

We use automated eligibility engines to confirm patient enrollment, plan benefits, and payer contracts before any service begins. Our system cross-checks each record against CMS and HHS guidelines to reduce denials. By verifying eligibility up front, we boost chart capture rates and keep your practice’s revenue cycle clean.

AAPC-certified coders review clinical notes, applying MEAT and TAMPER criteria to spot every hierarchical condition category. Diagnoses are mapped to the correct ICD-10-CM codes using the latest CMS code sets. Every code goes through peer review and a quality control check to protect documentation integrity and meet RADV audit standards. This step sharpens your risk score accuracy and supports fair capitation payments.

Once codes are locked in, our experts prepare the required CMS–HHS risk adjustment submissions, including CMS-2728 forms and supporting clinical documents. We file under HIPAA and NAAC rules, track reporting windows, and meet Quality Payment Program deadlines. This process reduces late-file penalties and strengthens your regulatory compliance.

Our robotic process automation (RPA) and natural language processing (NLP) tools scan charts to pull out key diagnoses and suggest HCC codes. AI-assisted abstraction flags missing conditions or inconsistent entries, cutting manual chart review time and raising accuracy rates. The system creates a full audit trail and delivers performance metrics that drive clinical documentation improvement.

You’ll get real-time dashboards on risk adjustment factor (RAF) trends, documentation gaps, and coder performance. We track KPIs such as RAF variance, chart conversion rate, and audit outcomes. With these insights, we help refine your coding workflows and close any revenue cycle gaps, so your practice meets quality metrics and maximizes reimbursement.
Why Choose J’S Vision as Your Risk Adjustment HCC Coding Company?
Here’s why so many health plans and provider groups trust J’S Vision for their HCC risk-adjustment coding:
Simplified Coding Through AI Assistance
We make coding less of a chore. Our AI-powered platform takes on chart abstraction and suggests the right codes so your team spends more time with patients and your risk scores get a boost.
Certified Human Oversight for Accuracy
Real expertise behind every suggestion. Every automated recommendation is reviewed by an AAPC- or AHIMA-certified coder who tracks the latest CMS guidelines to capture every condition accurately.
Triple-Layer Quality Review
Mistakes get caught early. Each chart passes through three layers of review peer check, manager audit and final quality validation so your RAF scores truly reflect patient complexity.
Flexible Review Models: Prospective & Retrospective
Flexibility to suit your workflow. Want to lock in HCCs before claims go out? We offer prospective reviews. Need to reclaim missed revenue? Our retrospective audits dig into past claims.
Seamless Integration, HIPAA Compliance & Scalability
Security and scale you can count on. We plug into any EHR, stay fully HIPAA compliant and flex our team size to fit a small clinic or a large payer.
Proactive Support & Continuous Improvement
A partner who grows with you. Your dedicated account lead checks in regularly, shares actionable insights and keeps our team trained on the latest coding guidelines.
Actionable Insights Through Real-Time Dashboards
Numbers you can act on. Interactive dashboards put your RAF gains, denial trends and coder productivity front and center so you can spot patterns and adjust in real time.
Trusted Partners
Relate is a better way to do sales and customer success for B2B SaaS startups

“The team at J’S Vision delivers our coding files on schedule with very few errors. We trust them for both outpatient and inpatient work so we do not have to double check. That saves us hours each week.”
Dr. Raj Malhotra Chief Medical Officer
“Working with J’S Vision feels like having our own coding department on call. They answer questions right away and update any files that need fixes. Their reliable service keeps our billing on track and makes audits smoother.”
Kara Simmons Practice Administrator
“J’S Vision handles our toughest cases such as emergency visits and long term care with skill and care. Their notes are always clear so we rarely have to ask for more detail. Our staff now spends less time on paperwork and more time with patients.”
Thomas Griggs Operations Manager
“With J’S Vision, audit flags are a thing of the past. Their coding is correct the first time and they turn around any revisions within a day. Our audit scores have gone up and we have real peace of mind.”
Lisa DuPont Compliance & Quality Officer
“The team at J’S Vision cleared our coding backlog and cut our billing cycle by two days. We have seen a steady rise in processed claims and a drop in manual rework. Our finance team loves their simple easy to read reports.”
Jordan Lee Billing and Claims Lead
Request a Free 30-minute Consultation With Our Risk Adjustment HCC Coding Specialists Today!
Some issues we can discuss are:
Existing risk adjustment HCC coding services and its process
Some common coding and billing errors
How can we improve coding accuracy through automation and software tools?
Ways to improve the accuracy of HCC scores and adapt to CMS guidelines
Food for your Thoughts




“J’S Vision’s accurate coding cut our claim denials by half, and it freed our billing team to spend more time on patient care. Their clear reports show exactly where to fix issues. We receive payment faster with fewer questions.”
Emily Tran Director of Revenue Cycle Management